February 4, 2026: N.J. Hospitals Deliver Nearly $35 Billion in Economic Impact and 162,000 Jobs
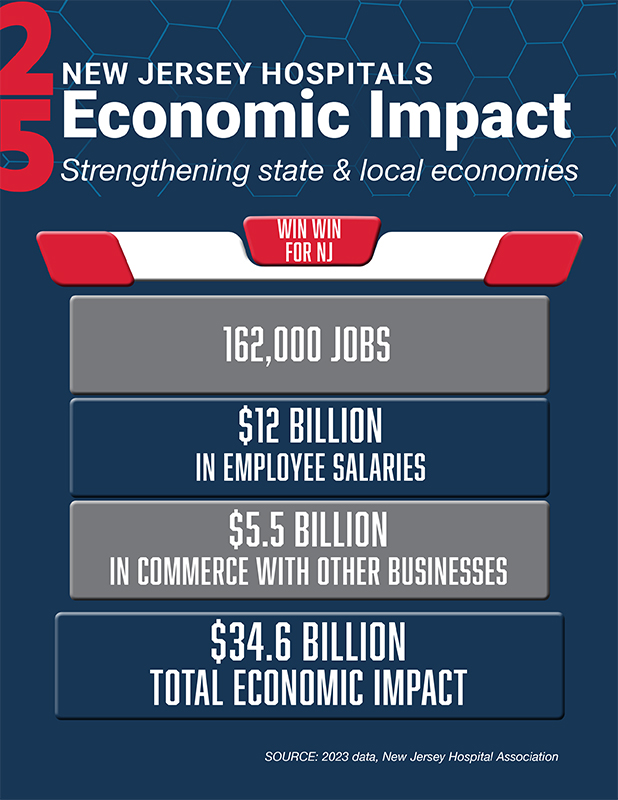 New Jersey hospitals are a cornerstone of the state’s economy, providing nearly 162,000 healthcare jobs and generating $34.6 billion in direct economic benefits.
New Jersey hospitals are a cornerstone of the state’s economy, providing nearly 162,000 healthcare jobs and generating $34.6 billion in direct economic benefits.
These findings come from the 2025 Economic Impact Report by the New Jersey Hospital Association, based on 2023 data from New Jersey’s 70 acute care hospitals.
“New Jersey hospitals are recognized for delivering world-class care, and their impact goes far beyond the bedside,” said NJHA President and CEO Cathy Bennett. “With 162,000 jobs and nearly $35 billion in economic activity, hospitals are economic playmakers for our state. To put it in perspective, the boost our hospitals provide in a single year is like hosting 10 World Cups right here in New Jersey.”
Additional contributions from New Jersey hospitals include:
- $5.5 billion in purchased services supporting other businesses
- $12 billion in hospital employee salaries; fixed labor costs represent nearly 60% of hospital budgets
- $664.8 million in state income taxes from hospital employees.
When factoring in hospitals’ purchases of goods and services and their support of businesses large and small, multipliers formulated by the U.S. Bureau of Economic Analysis push N.J. hospitals’ total economic infusion even higher.
- Each hospital job supports an additional 1.5 jobs in other sectors, turning 162,000 healthcare jobs into a total impact of about 398,000 jobs.
- Every dollar spent by a hospital generates $2.24 in economic output, contributing to $78 billion in statewide activity.
The full report, including breakdowns by hospital, county and legislative district, is available at: https://njha.com/economic-impact-report/.
Download the infographic.